Leaky Gut Syndrome
Leaky gut syndrome is repeatedly associated with other diseases, one example being autoimmune diseases. Scientists have been investigating the role of leaky gut in the development of diseases and how it affects our microbiome.
Contents
What is Leaky Gut Syndrome?
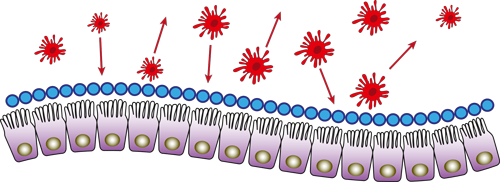
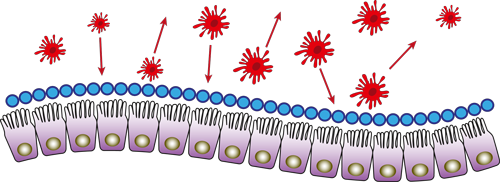
The term “leaky gut” refers to the increased permeability of the intestinal wall, which is an indispensable barrier between the body and the outside world. As a result, the mucus layer on the surface of the intestine changes and many bacteria simply die. Stress and inflammatory messengers are also produced, which destroy the intestinal cell layer underneath.
All toxic substances that enter the body with food are no longer simply excreted with the stool but can make their way unhindered into the underlying blood and nerve pathways and lead to corresponding changes and diseases. In addition to a balanced microbial colonisation of the intestine and sufficient formation of mucosal mucus and proteins of the immune system, an intact intestinal mucosa is indispensable for the defence against pathogens and to prevent the passage of unwanted substances through the intestinal wall.

Intestinal Wall - Protective Barrier
Due to its large total surface area, the intestine has many points of attack for pathogenic microorganisms. The so-called intestinal barrier, which consists of the healthy intestinal flora of the large intestine, the intestinal mucosa and the immune system located in the intestine, serves as protection and defence for the body.
Certain bacteria are able to produce substances that suppress the growth of harmful bacteria. Our intestinal bacteria are also responsible for regulating the protective function of the intestinal mucosa and the intestinal immune system. The intestinal mucosa has a particularly dense structure and, as the name suggests, is surrounded by a layer of mucus, which is intended to prevent the penetration of harmful germs.

Intestinal flora: symptoms and effects of dysbiosis
A dysbiosis (imbalance) is a change in the intestinal flora that is associated with pathological and often inflammatory symptoms. The causes of dysbiosis are very diverse.
Triggers can be, among others:
- Medication (e.g. antibiotics)
- Inflammation
- Overgrowth of pathogenic germs
- Nutrition
- Sweets
- Stress
- Interactions with the immune, nervous and hormonal systems
An imbalanced intestinal flora first becomes noticeable with symptoms such as burping, flatulence, bad-smelling stools or intestinal cramps. There is an imbalance of healthy and harmful intestinal bacteria. Pathogenic bacteria can multiply massively with corresponding changes in the environment and displace healthy intestinal bacteria. This leads to inflammation after a short time and subsequently to a so-called “leaky gut” syndrome.
Does an imbalanced gut cause tiredness?
If you are often tired and weary, even after a little exertion, there may be a condition behind it that still puzzles scientists: chronic fatigue syndrome.

Causes of Leaky Gut
It is very difficult to pin down one cause for the development of leaky gut. It is often an interaction of several components. Possible causes of leaky gut syndrome include:
- Medication: Medication, such as painkillers or antibiotics, can damage the intestinal barrier if taken continuously. Cortisone is another medication that can cause long-term damage to the sensitive lining of the stomach and intestines, leading to leaky gut.
- Allergies: These are becoming an increasingly common problem. Foods, metals, fungal toxins, dyes and artificial food additives can cause inflammatory reactions in the body. These inflammations also occur when the body reacts negatively to some foods with an intolerance and lead to damage to the intestinal mucosa in the body over time.
- Lifestyle: A stressful everyday life or regular alcohol consumption can also attack the gastrointestinal tract.
- Stress almost always plays a decisive role in many diseases. In the intestine, permanent stress also shows measurable changes in the intestinal mucosa. Studies have also clearly shown that regular consumption of alcohol can lead to damage of the intestinal barrier. On average, alcohol consumers are more prone to diarrhoea than people who live abstinent lives. Already abstaining from alcohol for a fortnight brings an improvement in the condition of the intestinal mucosa.
- Diet is also a relevant factor in determining the cause. An unbalanced diet or eating habits that are very high in sugar and fat can have a negative effect on the digestive tract and promote a leaky gut syndrome in the long run.
- Fungi: Our body is colonised by a variety of microorganisms, such as bacteria and fungi. These compete for balance and presence in the gut. Fungi are normally kept in check by good gut bacteria, but it can occur that there is an imbalance of this ratio and the fungi, for example, candida fungi, take over. Candida fungi are yeasts of the Candida group. Candida albicans is one of the best known of this type and is found in about 75% of all healthy people. As a rule, it does no harm, but in case of imbalance, it also plays a decisive role in leaky gut syndrome.
Consequences of a disturbed intestinal flora
As a result of leaky gut syndrome, the barrier function of the intestinal mucosa is impaired and there is an increased transfer of unwanted substances into the bloodstream. As already mentioned, these can be pathogenic germs, harmful substances or even large molecules from food.
First of all, inadequate responses of the immune system to these substances and germs are triggered in the intestine, which, among other things, cause allergic reactions to these substances and molecules. First and foremost, inflammations of the intestinal mucosa and, for example, food intolerances develop.
Based on these changes, chronic inflammatory processes subsequently occur, which can lead to autoimmune diseases such as type 1 diabetes or multiple sclerosis.
Today, the most modern laboratory analyses, which have revolutionised diagnostics, can clearly show the extent to which a reduced intestinal flora is the cause of a variety of disorders and diseases: this list ranges from allergies to chronic fatigue syndrome, chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis, depression to irritable bowel syndrome and colon cancer.

How is Leaky Gut Syndrome diagnosed?
One method of detecting leaky gut syndrome is the so-called lactulose-mannitol test. Here, the patient is given a lactulose-mannitol solution to drink and after a certain incubation period, the urine is examined for these substances. If there is an increased amount of these substances in the urine, then it is likely the intestinal barrier is weakened.
Another way to diagnose leaky gut is the zonulin test. This test checks the protein zonulin, which is secreted by the intestinal cells in response to certain stimuli and increases the permeability of the intestinal barrier. A serum sample is used to test how much zonulin is in the blood because an elevated level gives an indication of leaky gut syndrome.
A stool test can measure the inflammatory marker alpha-1-antitrypsin. This protein is largely produced in the liver and serves to regulate inflammatory reactions. If the intestinal barrier is increasingly permeable, alpha-1-antitrypsin can enter the intestine and ultimately be detected in the stool.
What to eat with Leaky Gut Syndrome
After the diagnosis of "leaky gut syndrome", the shock is deep, but the symptoms can be alleviated very well in a variety of different ways. The most important thing is to reduce the inflammation in the body, because leaky gut puts the body in contact with antigens, for example, wheat and cow's milk, which can trigger inflammatory reactions.
The first step would be to change your diet. This is often decisive for the intensity of the symptoms and can therefore be easily influenced with a well thought-out diet plan. Foods that are rich in refined sugar, unhealthy fats, preservatives and food additives favour a leaky gut syndrome or the development of other intestinal diseases if consumed over a longer period of time. This manifests itself in a permanent, "silent" inflammatory reactions in the intestine.
A balanced diet in the form of healthy fats, fibre, vitamins and minerals, soothes the intestines as well as inflammation. Especially in the case of proven food intolerances or allergies, poorly tolerated foods should be avoided.
The constant intake of food that causes turmoil in the intestines always leads to inflammation, which promotes diseases such as Crohn's disease or ulcerative colitis. A high-fibre diet with oats, rye or vegetables and fruit are very good for the intestinal flora and positively influence digestive activity.

How do I manage Leaky Gut Syndrome?
In addition to dietary changes, there are other therapies that can help alleviate the symptoms and make living with this diagnosis easier. However, it is important to choose the appropriate medication only in consultation with your doctor. Another possible therapy approach is that with probiotics.
According to the World Health Organisation (WHO), probiotics are “viable microorganisms which, when administered in sufficient quantity, have a health-promoting effect on the host“. In this case, the host is considered to be the human being who ingests the microorganisms. Probiotics contain bacteria that are naturally present in the human intestine and therefore support the activity of the bacteria already present. Often there is an imbalance of good and bad bacteria in the intestine when a leaky gut syndrome is present. Therefore, a supply of viable, probiotic intestinal bacteria is important for the restoration of a healthy intestinal flora.
What probiotic should I take for Leaky Gut Syndrome?
Ideally, a combination of specific, probiotic bacterial strains that have been shown to be able to reduce excessive permeability in the intestinal mucosa should be considered.
Probiotically effective bacterial species for leaky gut syndrome are, for example, Bifidobacterium longum, Lactobacillus acidophilus, Lactobacillus plantarum, Lactococcus lactis and Lactococcus lactis. The dosage and duration of intake in turn depends on various aspects: Age, possible underlying diseases, diet, mental and physical impairments, smoking, alcohol, various (drug) therapies, etc. A detailed consultation with a doctor or in a pharmacy will provide detailed information on which probiotic or which combination of probiotic bacterial strains is the best solution.
Any questions? Contact us!
Our highly-qualified consultant team is made up of doctors, pharmacists, biologists, nutritionists and microbiologists. Contact us to get advice regarding our products, your intestines, as well as your microscopic inhabitants.

Help & Advice
Institut AllergoSan
EU
OMNi-BiOTiC® − Blog
Stay informed!
Read more interesting articles about our gut and get tips for your gut health!
OMNi-BiOTiC® − Blog
Stay informed!
Read more interesting articles about our gut and get tips for your gut health!
OMNi-BiOTiC®
Our intestinal bacteria perform at their best every day. Unhealthy diets, stress or medication can change our intestinal flora. The targeted supply of specially selected strains of bacteria – called probiotics – supports our intestines in every phase of life: while taking antibiotics, in particularly demanding times or as a daily go-to for the whole family.
OMNi-LOGiC®
The intestine is the health centre of our body: billions of intestinal bacteria work every day to ensure that digestion and the body’s defences function optimally. In order for these useful helpers to feel at home and fulfil all their important tasks, they need specific dietary fibres as a food source, such as those contained in prebiotics.
META-CARE®
Many individuals struggle to obtain sufficient vitamins, minerals, and trace elements through their diet. Additionally, particularly during periods of elevated stress and heightened mental or physical strain, the body’s demand for nutrients intensifies. The body’s functions can be aided by taking high-quality micronutrients and plant extracts, enhancing your overall health and well-being.
OMNi-BiOTiC® − for a good gut feeling every day
The secret of OMNi-BiOTiC®’s success lies in its innovative formulation and high-quality standards. These are top priorities in developing probiotics and ensuring tangible benefits for users.

















