Gut Flora
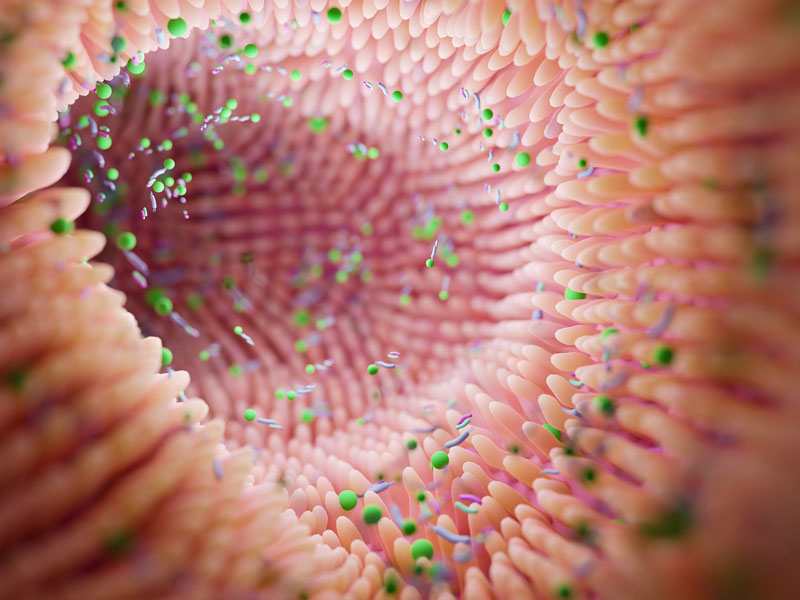
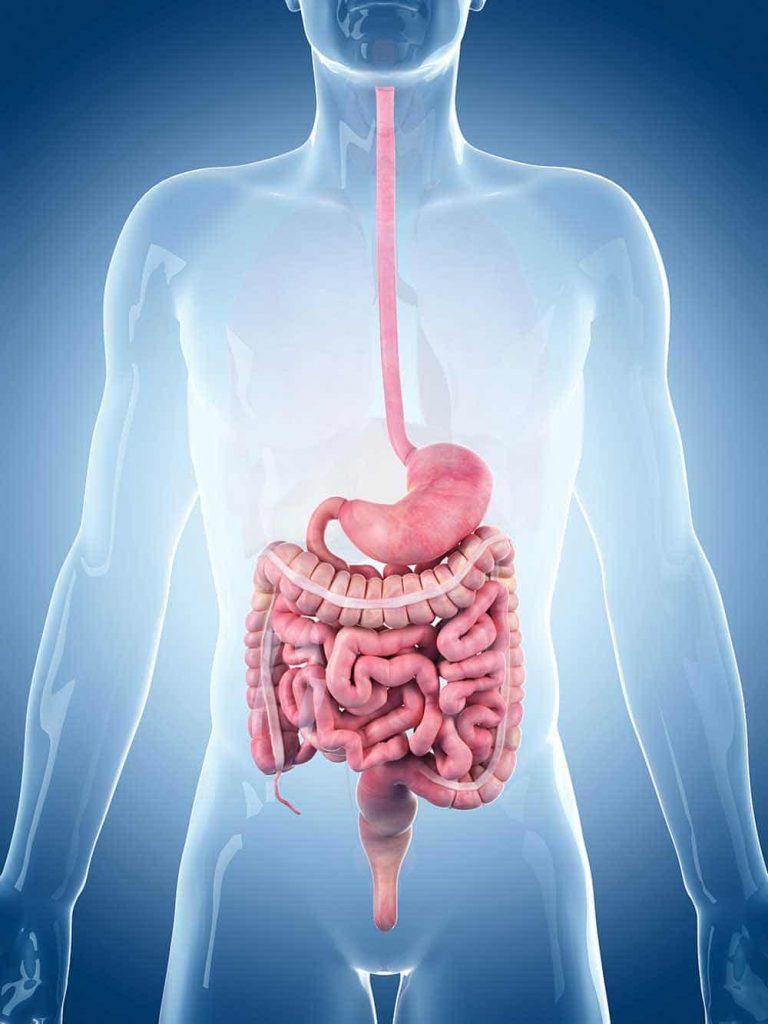
The intestine is the centre for many important processes in the body that are essential for human health. It performs vital tasks, but it needs the help of its tiny inhabitants. There are trillions of them in the human intestine: the bacteria. They are microorganisms and live primarily in the large intestine. Together – i.e. in their entirety – they are called “intestinal flora“. However, the term “flora” is no longer appropriate, because it is still based on the old view that the microscopic living organisms are counted among the plants. The special feature of the intestinal flora is its importance for the immune system.
Contents
Development of the gut flora
How does the bacteria get into our intestines?
A healthy intestinal microbiome (intestinal flora) in our digestive tract forms the basis for our general well-being. The colonisation of the intestine with beneficial bacteria and other microorganisms only begins with birth. The colonisation depends on whether the birth happens vaginally or with a caesarean section.
In a vaginal birth, the babies come into contact with the mother’s vaginal flora, which has a significant impact on the baby’s microbiome. With a caesarean section, on the other hand, more skin germs and hospital germs are found in the children. This is why the risk of contracting diseases is significantly higher in C-section babies than in those born during a vaginal birth. Above all, it should be mentioned that in the case of a caesarean section, antibiotics are usually prescribed to the mother as a preventive measure. This has a further negative effect on the bacterial flora of mother and child.
What does breastfeeding have to do with bacteria in the child's intestine?
After the child is born, the intestinal flora is far from “finished”. It can continue to mature until several weeks after birth. With the feeding of breast milk, further bacteria are transferred from the mother to the child. The transfer already begins with the skin, when the child drinks from/out of the breast and thus the bacteria are already taken over by the skin microbiome. The germs enter the breast and thus the milk via the milk ducts.
According to the latest knowledge, it is discussed that an endogenous transfer of bacteria from the maternal intestine via the lymph-blood system into the breast milk takes place. According to this, breastfed children contain the optimal prerequisite for the development of an optimal intestinal flora.

Your gut flora during pregnancy
Our intestinal flora also plays a central role in pregnancy, from conception to birth. Via a “mucosal path”, the beneficial lactobacilli that keep your intimate area healthy reach their destination from the rectum and settle there permanently. These lactic acid bacteria not only keep the vaginal area healthy and displace unwanted fungi and germs, but they are also of great importance during conception.
Structure of the gut flora
The intestine of a healthy adult is colonised by about 100 trillion bacteria. These are very important for our body, as they are responsible, among other things, for the production of important vitamins (e.g. vitamin K), hormones, amino acids and short-chain fatty acids for the intestinal mucosa.
Interestingly, this enormous number of bacteria is composed of only 500-1000 different bacterial species, which in turn are divided into 4 different divisions, so-called “phyla”: Firmicutes, Bacteroidetes, Proteobacteria and Actinobacter.
Over 99% of these bacteria are anaerobes, which means that they need an oxygen-free environment to survive. This may sound surprising at first, but on closer inspection, it is logical, since the intestine, with its length of dozens of metres, actually contains no oxygen inside.
Just like humans, bacteria are true adaptation artists and know exactly where they have to settle in order to live optimally. The different types of bacteria are therefore distributed in different ways throughout the gastrointestinal tract.

Small intestine
- Longest part of the digestive system
Only a small part of the entire intestinal flora is located in the small intestine. The best-known representatives are found in this section of the intestine: Lactobacilli such as Lactobacillus acidophilus ensure the maintenance of the appropriate pH value here through the production of lactic acid.
If the pH value in the small intestine tips, this can result in an outbreak of pathogens (intestinal fungi!). These lactic acid bacteria are therefore an integral part of a functioning immune system – a displacement (possible through a very salty diet) has serious consequences.

Large intestine
- Last part of the digestive tract
The bacteria found in the large intestine ferment dietary fibre into important micronutrients. A prominent probiotic bacterium of the flora located in the large intestine is Bifidobacterium bifidum. This non-motile (=local) bacterium is one of the “all-rounders” of the intestinal flora of a healthy adult.
High-quality studies prove a role of Bifidobacterium bifidum in the prevention of irritable bowel syndrome, chronic inflammatory bowel diseases, stabilisation of cholesterol levels, improvement of allergic symptoms and skin appearance, as well as psychological stress, protection against free radicals and even a possible role in the development of colon carcinomas.
Bifidobacterium bifidum, along with other important probiotic germs found in the colon, such as Bifidobacterium breve, Lactobacillus brevis, Enterococcus durans or Lactobacillus rhamnosus, belong to the so-called “leading bacterial strains” – this means that they are essentially involved in the healthy build-up of a functioning intestinal flora, and can ensure that important other bacteria can also multiply in the intestine.
The multitude of bacterial strains explains why the ecological balance in the large intestine in particular reacts very sensitively and this weakness is reflected in daily practice in the form of dysbiosis.
Skin & Gut Flora
How do our gut bacteria influence our skin?
“Our skin is the mirror of our soul” is a well-known saying that is often used with good reason. If we are not emotionally well, this is often unconsciously expressed in our skin. The skin looks pale and can develop pimples or redness. Why does this happen and what role does the intestinal flora play?
Functions of the gut flora
When microorganisms were first discovered in the intestines, they were thought to be a disease and named “intestinal toxaemia”, meaning “poisoning of the intestines”. After all, bacteria were known and feared as pathogens. With special colon cleanses or even surgical removal of the colon, some doctors tried to expel the “dangerous” bacteria.
In the meantime, it has been established that the intestinal flora is not harmful to humans, but very important. Some food components could not be utilised at all or not completely without the intestinal bacteria. In addition, the microorganisms of the intestinal flora have other important functions:
- Contribute to the functioning of our immune system.
- Partly form vitamin K, which is important for blood clotting.
- Contribute to the energy supply of the cells and the intestinal mucosa.
- Break down harmful substances, e.g. cancer-promoting substances.
- Prevent pathogens from multiplying in the intestine.

What causes the gut to become imbalanced?
The intestine and the intestinal flora are a complex and independent ecosystem in which a large number of different species live. Since the environmental conditions in the intestine remain constant, at least in healthy people, this ecosystem is usually relatively stable.
However, there are factors that can negatively influence the composition of the bacterial colonisation.
Diet & Lifestyle
- For a healthy gut
Your diet has a significant influence on the gut microbiome. Food components, especially dietary fibre, serve as a source of nutrients and energy for the microorganisms.
Scientific studies have long shown that there is a connection between dietary habits and the condition of the intestinal flora. It was also found that the intestines of overweight people are not only dominated by different types of bacteria than those of normal-weight people but also have fewer species.
Medication
- Good intentions with consequences
This mainly refers to treatment with antibiotics. These are drugs that either inhibit the growth of bacteria or destroy them. When fighting bacterial infections, the administration of antibiotics is usually necessary. But these antibiotics not only destroy pathogens but also entire strains of the “good” intestinal bacteria.
Is the intestinal flora to blame for the development of some health conditions?
An altered microbiome is associated with gastrointestinal diseases, obesity, diabetes, atherosclerosis and depression.
Today we already know that the bacterial balance in our body is to blame for many everyday complaints, such as bloating or feeling full. A healthy intestinal flora is therefore the most important factor for general well-being.
Healthy Gut Flora
To keep the intestinal flora in balance, we recommend the following:
Aim to maintain a balanced diet
DO’s
- High-fibre foods such as carrots, peppers, blueberries or raspberries, cabbage, fennel and pulses such as chickpeas, beans or lentils.
- Take time when eating: Sit down and chew thoroughly
- Gentle preparation (steaming, light cooking)
- Whole-grain products: keep you full longer and stimulate the intestinal muscles
- Drink plenty of water
DONT’s:
- Sugary drinks and alcohol
- High-fat or high-sugar foods
- Deep-fried food
Probiotics and Prebiotics:
Probiotic bacteria are living microorganisms that bring health benefits to humans when they enter the gut in sufficient quantities. There are a variety of different specific probiotic bacteria that cause detectable, positive effects in the human intestine.
In order to maintain the important biodiversity of the intestinal bacteria or to create optimal conditions for the intestinal inhabitants, there are two possibilities: firstly, the supply of food for the “good” intestinal bacteria in the form of prebiotics. These are soluble dietary fibres such as pectin, inulin and oligofructose.
These are found in numerous foods, for example in legumes, certain vegetables or nuts, but can also be specifically supplied in sufficiently high doses through prebiotics products.
The second option is to take probiotics to displace the harmful bacteria and balance out a dysbalance in the microbiome. Here, too, selected products should be used that meet strict quality criteria and whose benefits for human well-being have been proven in scientific studies.
COVID-19:
Patients often have an imbalanced intestinal flora
A coronavirus (COVID-19) infection often causes changes in gut flora, the extent of which was associated with disease severity in a study in Gut (2021; DOI: 10.1136/gutjnl-2020-323020). COVID-19 is primarily a respiratory disease. However, coronavirus can also infect the cells of the intestinal mucosa. The intestine is also the body’s largest immunological organ, whose job is to control intestinal bacteria. Since there is often an overactivity of the immune system in severe COVID-19, an influence on the intestinal flora is conceivable.


















